Executive Summary
Healthcare costs are rising in the U.S. According to the Centers for Medicare & Medicaid Services (CMS), National Health Expenditure increased 4.6% in 2019, reaching $3.8 trillion, with Medicare spending climbing 6.7% to $799.4 billion.1 Meanwhile, U.S. Census Bureau estimates show a growing 65-and-older age group, which increased 34.2% between 2010 and 2019.2 Among this group, the Lown Institute reports that 42% take at least five prescription medications.3
Rising healthcare costs and a growing elderly population could have significant implications when it comes to adverse drug events (ADEs). ADEs occur when an individual is harmed by medication, even when that medication is used appropriately. They are responsible for around 1.3 million emergency department visits a year, and roughly 350,000 individuals require hospitalization for additional treatment.4
Tabula Rasa HealthCare’s (TRHC) MedWise Risk Score™ is a novel approach to help clinical pharmacists target patients at risk for ADEs. Used together with TRHC’s clinical decision support technology, MedWise® Science, pharmacists can identify those patients with high risk scores and target them for risk-mitigating interventions. TRHC has found these pharmacist-led interventions to result in better patient outcomes, including reduced falls, hospital admissions, emergency department visits, medical expenditures, and deaths. Pharmacists and other healthcare providers working with TRHC clinical pharmacists can use these technologies to effectively pinpoint risk, identify medication-related problems, and make recommendations that advance patient outcomes and ultimately save lives. The impact of clinical pharmacist-driven interventions, under the scope of medication safety reviews, using these technologies is further illustrated in a new peer-reviewed research series in The American Journal of Managed Care.
Understanding MedWise and the MedWise Risk Score
TRHC’s MedWise Risk Score helps pharmacists determine which patients are at risk for ADEs1 by analyzing medication-related risk factors through proprietary algorithms.2 Unlike traditional medication therapy management offerings, which evaluate a number of chronic diseases, number of medications, and Medicare Part D costs, the MedWise Risk Score evaluates pharmacokinetic and pharmacodynamic characteristics of active medication ingredients.3 This evaluation incorporates over-the-counter medications, herbals, and supplements to illuminate simultaneous, multi-drug interactions.5 Based on the data, patients are assigned a risk score ranging from 0 to 50, where 0–9 indicates minimal risk, 10–14 indicates low risk, 15–19 indicates intermediate risk, 20–29 indicates high risk, and 30 and above indicates severe risk.6
In the CMS Innovation Center’s Enhanced Medication Therapy Management (EMTM) model, TRHC clinical pharmacists used the MedWise Risk Score with MedWise Science, a clinical decision support technology, to optimize patient outcomes.7 The MedWise Matrix creates a visualization of a patient’s complete medication regimen and enables pharmacists to identify and address medication-related problems that can lead to ADEs.
Identifying Patients with Higher Risk for Negative Outcomes
Research has proven that MedWise Risk Scores can help pharmacists successfully identify patients whose medications—when used together—put them at greater risk for negative outcomes including ADEs, falls, higher medical expenditure, emergency department visits, hospitalizations, and death. A study by Michaud et al. included over 200,000 participants who were prescribed medication in 2018.6 A MedWise Risk Score was calculated for the year 2018 and, according to the data, there was a greater percentage of intermediate, high, and severe max scores among participants who had at least one ADE. Specifically, 18.6% of participants with one or more ADE had an intermediate score, 26.5% had a high score, and 9.9% had a severe score.
The results also showed a strong link between the MedWise Risk Score and falls. Compared to participants with a minimal max score, participants with a severe max score were most likely to experience a fall, followed by participants with a high max score, then an intermediate max score.
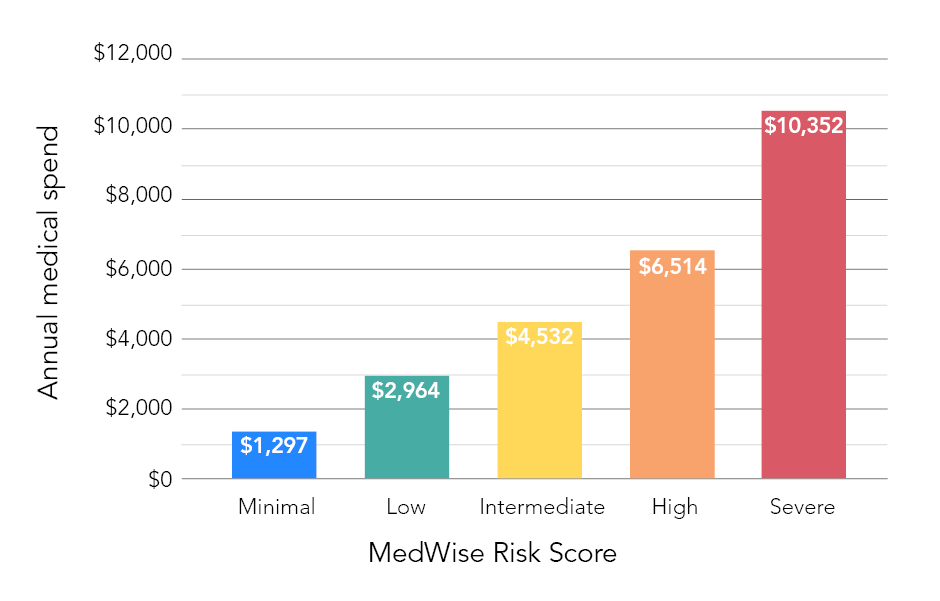
Data trended similarly for medical expenditures. Fifty percent of participants with a minimal max score had a mean yearly medical expenditure of $1,297. This cost escalated to $2,964 for participants with a low score; $4,532 for participants with an intermediate score; $6,514 for participants with a high score; and $10,352 for participants with a severe score (see Figure 1).
In addition, the data revealed associations between the MedWise Risk Score and emergency department visits, hospitalizations, and deaths. For example, the data showed a greater number of participants with high and severe max scores among those who died compared to those who remained living. These results confirm the MedWise Risk Score’s ability to identify which patients have the greatest risk for negative outcomes.
Pinning Down Medication-related Problems
By identifying patients with the greatest risk, a MedWise Risk Score helps to prioritize individuals for MedWise Safety Reviews. These reviews enable pharmacists to leverage the clinical decision support tools to detect medication-related problems and make recommendations to prevent dangerous drug interactions.4
Pharmacists used MedWise Risk Scores and MedWise Science to effectively lower patient risk for multi-drug interactions in a study by Bankes et al.7 During the study, analyzing MedWise Risk Scores helped pharmacists prioritize 22,696 high-risk participants for their first-ever review. Guided by MedWise Science, pharmacists detected 36,455 clinically actionable medication-related problems, roughly 85% of which were adverse drug reaction, drug interaction, and unnecessary medication use. MedWise Science also informed pharmacist recommendations to address the medication-related problems, with start alternative therapy, discontinue medication, change time of medication administration, and change dose topping the list. According to the study’s results, pharmacist recommendations could reduce the average MedWise Risk Score by 4.7 points.
Improving Patient Outcomes
Insight from MedWise Safety Reviews can optimize prescribing practices and impact patient outcomes. This impact was proven by Stein et al., who studied the impacts of MedWise Safety Reviews on medical expenditures, hospitalizations, emergency department visits, and mortality.5 The research included two groups totaling 11,436 participants: 4,384 individuals who received their first-ever review in 2018 and at least one review in 2019, and 7,052 individuals who did not receive a review. According to the data, participants who received MedWise Safety Reviews benefitted from less total medical expenditure as well as fewer hospitalizations and emergency department visits, comparatively.
While mean total medical costs (Medicare Part A and Part B) increased for both groups from 2018 to 2019, participants with MedWise Safety Reviews saved in comparison. In fact, the findings revealed an 8.5% increase for those who received MedWise Safety Reviews versus a 16% increase for those who did not, resulting in 7.5% cost savings for those who completed reviews. Similarly, emergency department visits increased in both groups, but this increase was less among participants with MedWise Safety Reviews. According to the data, the change from 2018 to 2019 was 2.3% for those who received MedWise Safety Reviews and 12.6% for those who did not, marking a 10.3% decrease for the intervention group (see Figure 2).
Meanwhile, the hospitalization rate decreased among participants who had MedWise Safety Reviews, but increased among participants who did not. Hospitalizations climbed 6.6% for those who did not complete reviews but dropped 3.4% for those who did, resulting in an overall 10% reduction for those who completed reviews (see Figure 2).

The data also demonstrated impact in terms of mortality. While 6.8% of participants who had their first-ever review in 2018 died by the end of 2019, 8.9% of participants who did not have a review died by the end of 2019. This marks a 2.1% difference between the groups (see Figure 2).
Putting Results in Perspective
With over 6 billion prescriptions dispensed in 2020, the safe use of medication is critical.6 Advanced tools like MedWise Science and the MedWise Risk Score are important tools, helping to shed unparalleled light on medication regimens and prescribing practices. Research has proven the MedWise Risk Score effective in identifying patients whose medication regimens put them at greater risk for negative outcomes. For high-risk patients, pharmacists can pinpoint medication-related problems and recommend measures that reduce risk through pharmacist-led consultations, which leverage MedWise Science.
As research demonstrates, this strategy ultimately leads to improving the safety of medication use and better patient outcomes. Given overarching trends surrounding healthcare costs, the elderly, and ADEs, wider use of advanced clinical decision support technology, such as MedWise Science, can help clinicians significantly improve the healthcare landscape.
Share this: